Molluscum Contagiosum
What is Molluscum Contagiosum?
Most often seen in children, molluscum contagiosum is a common viral infection. This virus affects the outer layer of skin and does not usually move through the body. The firm, skin-colored bumps that develop from molluscum contagiosum usually disappear within a year on their own but doctors often recommend treatment to keep the virus from spreading. Molluscum contagiosum can appear in adults and, if it involves the genitals in the adult cases, it is considered a sexually transmitted disease. People with weakened immune systems are more susceptible to the virus as well.

What are the signs and symptoms of Molluscum Contagiosum?
Generally, molluscum contagiosum produces little white, pink or flesh-colored bumps that have a dimple or pit in the center. In most people, the growths range in size from about two to five millimeters in diameter. Molluscum contagiosum often appears on the face, neck, abdomen, arms, legs, or genitalia.
What are the causes of Molluscum Contagiosum?
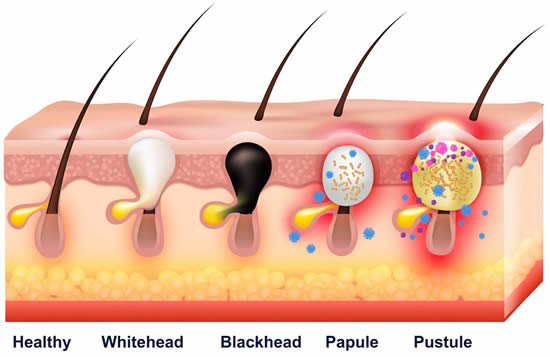
The molluscum contagiosum virus, a member of the poxvirus family, enters your skin through hair follicles, pores, or abrasions on the skin’s surface. Highly contagious, the virus spreads by person-to-person contact, sexual contact with an infected partner, or through contact with contaminated objects like toys, door knobs, or faucets. Scratching, rubbing and shaving the papules can spread the virus to other areas of skin.
What treatments are available at the dermatologist for Molluscum Contagiosum?
Your doctor will need to destroy the infection-causing cores inside the papules. Once this core is destroyed, the infection will heal. Several methods can be utilized to eliminate these cores:
- Chemical agents to remove the infected skin
- Cryotherapy to freeze the areas and kill the infection
- Curette, scalpel, or other cutting device to surgically remove them
- Lasers to destroy the infected cells

FAQ About Molluscum Contagiosum
Is molluscum contagiosum contagious?
Yes, molluscum contagiosum is contagious until all the bumps have gone away. The virus can be spread from one part of the body to another or from one person to another through direct contact with the bumps or objects that have touched them.
Is molluscum contagiosum dangerous?
No, molluscum contagiosum is not dangerous in most cases. It is a mild and harmless infection that does not cause serious complications. However, it can cause discomfort, embarrassment, or anxiety for some people. It can also interfere with sexual pleasure or intimacy. In rare cases, it can cause secondary infections, eye problems, or widespread lesions in people with weakened immune systems.
Can molluscum contagiosum recur?
Yes, molluscum contagiosum can recur if a person is exposed to the virus again. The infection does not provide immunity against future infections. Therefore, it is possible to get molluscum contagiosum more than once in a lifetime.
Is there a dermatologist near me in Boise City that offers treatment for molluscum contagiosum?
Yes. At our Boise City dermatology office we offer treatment for molluscum contagiosum to patients from Boise City and the surrounding area. Contact our office today to schedule an appointment.